I am describing our emotions, they are up and down and all around. So much has been going on medically in the last three years, but more in the last six months. Lucy’s motility, the way her GI system moves food, meds, and stool through her body has been declining rapidly in the last six months, but even more so in the last two months. Really I don’t have the energy tonight to go into too much detail, so I will skim over what we have been thinking about and dealing with recently. As many of you know in addition to being 100% TPN dependent Lucy has a gj-tube, we use the j port of her tube to give her meds and very small amounts of feeds, and we use the g-port to drain her stomach 24/7. We drain her stomach because she can not tolerate having anything in her stomach. It was our hope and desire when we started Lucy on TPN back in October that her belly would wake-up so to speak, and she would be able to start tolerating feeds again. This hope is no longer a reality, at this point none of her doctors believe that Lucy will ever get off of TPN. It is believed that Lucy will not be able to take in enough nutrients via her GI tract and therefore TPN is necessary to keep her properly nourished and hydrated. Some of you may have already come to this conclusion, but as parents it is not an easy reality to accept. Perhaps by me writing this it will sink into my heart, as I do comprehend the science behind all of this, it’s the emotional stuff that takes more time to process these days.
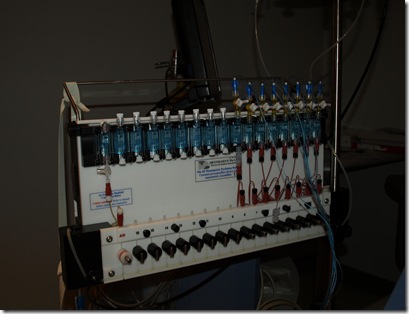
We are having problems with Lucy’s gj-tube. Specifically we are having a terrible time placing them and having them stay in the right spot in her intestines. A typical tube placement should last three months, then you call IR and schedule a tube change. We are going on tube number ELEVEN in ten weeks, but even worse we are going on tube number three this week alone! Lucy’s motility is so poor it is moving backwards, pushing things back into her stomach. In medical terms this is called reverse peristalsis, peristalsis is the movement of the GI tract, it should move down and out if you know what I mean. In addition, Lucy’s belly does not empty well as she suffers with delayed gastric emptying or gastroparesis, which has progressed as well. When we attempt to place a gj-tube in Lucy part of our struggle with placement is getting her stomach to empty so that they can thread the tube into her jejunum. Once placed, her motility is working against us and pushes back the tube that was just placed. On Monday we witnessed this on x-ray after spending quite a bit of time trying to place a new tube.
What’s a mama to do? Good question, after her tube placement in IR and the radiologist giving me a look like how many more of these are you going to put her through, I marched on over to our main doc’s office and shared with him what we had just witnessed and then picked his brain some more about a motility test that Drew and I have seriously been struggling with making a decision about. Why do we keep trying to force feeds? The simple answer according to Dr. R, “if you don’t use it, you’ll loose it!” Coating the bowel wall with even the tiny amount of food that we are feeding Lucy is the best way to keep the bad bacteria from taking over. We are at war with the bacteria in Lucy’s GI tract, and at the present time we are fighting three pretty potent bowel bacteria and yeast. How are we going to med and feed her if we can’t keep the hardware in her that we need to do this? Another excellent question, and this is where we stand at the present time. Dr, R is talking with a GI specialist out of the area that works with one of his small bowel transplant kids, this GI has done a procedure in which they place the j-tube endoscopically and secure it to the bowel wall with a clip of sorts. We are not even sure that this could be an option for Lucy, but at this point we need to think way outside of the box. A surgical j, where surgically a separate hole for a j-port is made some where along the jejunum, is just not an option for our girl because there are too many risks involved with the procedure. Lucy has intestinal myopathy, her muscles in her intestines are floppy and are deteriorating. Preforming a surgery in which you rearrange the intestinal wall is extremely risky in a kiddo like ours.
I mentioned above that Drew and I have been thinking hard about a motility study that may or may not yield some information about how the nerves and muscles function in Lucy’s stomach and small bowel. Our new GI at CHOP who specializes in motility disorders said to us in February that he can not make any recommendations for Lucy until after she undergoes an antrodoudenal manometry study. It is an invasive study, that may or may not yield valuable information… how’s that for clarity. Our little one is complicated, and so is this study, two complicated issues make for one extremely complex situation. We have many things we need to consider and do to prepare Lucy for the study. A few of which include having an upper GI done next week to even determine if we can do the study, and… oh yeah… our main doc being out of the country while Lucy is scheduled to undergo this study, stress on top of stress…that seems to be our family motto.
I know I stated in the beginning of this post that I was only going to skim over the issues…well, I did. The issues together are so complex that it is impossible to write about them in one post, so look forward to future posts in which I will try and dissect the matters into easier to digest pieces(pun fully intended).