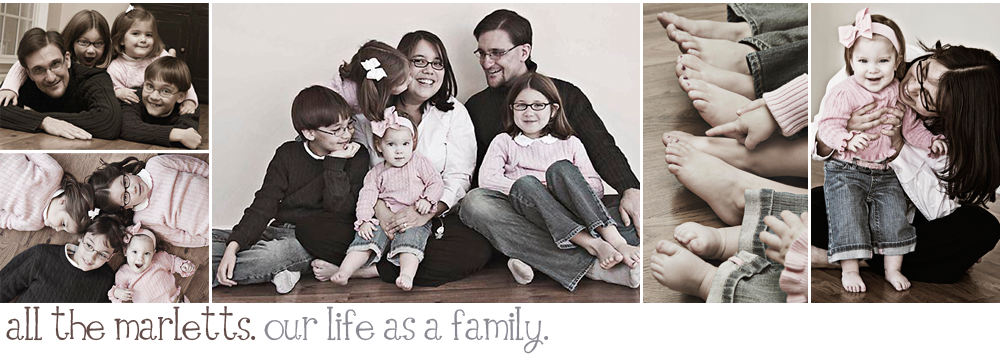
I want to say a heart felt thank you to those of you who continue to check on, think of, pray for, and love all of the Marletts. We value and appreciate all of the love and support, and thoughts and prayers that are given to our family. I am continually in awe of people! Despite what the media portrays, people are good, they genuinely care! They are loving and want to lend a helping hand. People want to understand and relate, we are witnesses to all of this every day!
I have wanted to write so many times in the past few weeks, but as it should be life has gotten in the way, it happens. The need for sleep outweighs everything at the moment. We have also needed time to try and process all that has and is occurring, time is not something that is in abundance around here. I am proud to say that we have fallen into somewhat of a groove with things at home, it feels so good to have a sense of routine and familiarity back - once again, we have a new normal. That being said, we know that this is only temporary as Drew and I have been contemplating, praying, thinking about, and discussing with our medical team just what we are going to do about our girl and her failing gastrointestinal system.
I mentioned when we left the hospital at the beginning of March (can you believe we have been home since then, with the exception of a few clinic visits :) that we are facing some very difficult choices when it comes to Lucy's life. We all felt that with the placement of a somewhat permanent biliary stent, and by permanent I mean eight weeks, and the use of continual "big gun" IV antibiotics and anti-fungals that we had some time to go home and think about these difficult choices. Eight weeks goes by faster than you think, and so now here we are, faced with the reality that we need to do something.
Let me just preface this post with saying that our options for Lucy are not going cure her or even make her better. The choices that we are contemplating will hopefully reduce her risk of recurrent life threatening infections, which in turn will hopefully minimize some of her daily pain, thus improving her overall quality of life.
All that being said, we really only have two options for Lucy. The first, is maximally invasive surgery to try and reconstruct her bile duct, and the second is to do nothing. Both options come with a tremendous amount of risks!
If we choose to do nothing, what we are really choosing is to have the stent removed and treat the reoccurring
cholangitis and pain that will ultimately ensue. It is thought that Lucy will develop a stricture either upon stent removal or soon there after. Stenting her bile duct did nothing to correct the reason why Lucy needed a stent in the first place, unfortunately it was a temporary solution to a much bigger problem. Even though we would love to keep the stent in for as long as possible, it poses an even bigger risk of infection for her the longer it stays in, especially if it becomes embedded in the wall of her bile duct which is a risk of leaving it in longer than the recommended eight weeks. We will keep her on continual IV antibiotics and anti-fungals all in an attempt to keep the "bad guys" away for as long as possible. But here's our reality, these medicines can only fight off specific types of bacteria and fungus. Eventually, when you fight with the bug kingdom as much as we have, these meds loose their ability to fight off bacteria because the bacteria become resistant to them. Equally as worrisome is the fact that Lucy will be in even more pain, because an occluded bile duct hurts.
Dr. R very lovingly shared with Drew and I that doing nothing and letting her body do what it ultimately will do most likely means that she will suffer a very painful end of life in which she will need to be heavily medicated to remain comfortable. His concern was for us as well, sharing with us that we will have to make some very tough decisions as her parents all in an effort to not prolong her suffering. These conversations, though very difficult, are our reality these days.
Our other option we have for our girl is maximally invasive surgery in which we will reconstruct her bile duct. Two of the brightest surgery minds at DuPont have been working hard to figure our just how exactly we can go about doing this. One of these brilliant minds is our surgeon Dr. K who knows and loves our girl, and the other brilliant mind is the liver transplant surgeon Dr. D who has a reputation for doing the impossible. Don't think for one moment that we don't know how lucky and blessed we are to have the outstanding medical team that we have!
The tried and true surgical method for reconstruction of a bile duct is to do what is know as a heptocholangiojejunostomy
Roux en Y (not only can I spell it, I know what it is:). Very simply, this is a complex procedure in which the surgeon takes a portion of jejunum, brings it up to the liver creating a Y of sorts. Then attaches it to the liver creating a new conduit for bile to drain. The bile from the liver then flows directly into the small bowel.
This option, though tried and tested, is a very very scary operation for our girl. Her intestines are coated in every type of bad bacteria and fungus. If we were to connect Lucy's jejunum to her liver we all fear that we would be putting her at an even greater risk for infection. In fact both Dr. K and Dr. R believe that she will very likely develop sepsis immediately upon connection, if not then soon thereafter. Although Lucy has survived sepsis before, this time we are fearful that the bacteria in her small bowel are more potent than the meds we could use to treat it.
Are you gasping yet?
Breath, we are not going to be able to fix Lucy's bile duct this way, the risks do not out weigh the benefits. Instead we are seriously considering an alternative surgical procedure, alternative as in has never been done before. This procedure will involve resecting either a portion of her jejunum or using her diseased gallbladder to create a conduit which will attach to her liver creating a new bile duct of sorts. Instead of connecting the conduit to her diseased small intestine, we will instead create an
ostomy, or a hole (I know, as if the girl doesn't have enough holes in her body already) on the the exterior of her body in which the bile from her liver will drain via gravity into an ostomy bag. The reason we want to create an ostomy is so that we can eliminate any risk of infection coming from the bacteria in her small bowel. If the conduit or new bile duct is not connected to her small bowel then in theory bacteria from her small bowel will not be able to infect her liver, thus minimizing her risk for ascending cholangitis.
This option gives Lucy the lowest risk of infection, if it works! However, the procedure itself is massive and as such comes with a tremendous amount of risks, the biggest being that she may not recover! We also understand that an ostomy is no picnic, especially since we are going to have to attempt to keep her ostomy sterile. Ostomys are typically anything but sterile. Ideally we would all love if this procedure could be done
laproscopicly which will minimize her recovery time, but that is something that has yet to be determined. The two surgeons differ on what organ they want to use as the conduit, but both agree that no matter what organ is used this surgery has the potential of reducing Lucy's risk of reoccurring ascending cholangitis. Any surgery is a risk, but one of this magnitude on our girl brings new meaning to the word.
Which way are we leaning... well, that all depends on when you ask me. We do realize that there is no right or wrong decision here, what we ultimately end up choosing to do for our girl will be the right decision no matter what! If I were to sum up our biggest fear, it would be the fear of doing more harm than good. Our goal is and remains to give our girl the best longest life!