Sorry to leave you all hanging…for some reason I had difficulties posting on our blog from the hospital network. When all was said and done it was nearly 7:00pm when we rolled out of there. It was a loooong day(we woke up at 4 am) and by the time we came home, picked up our other three children, infused meds, got everyone ready for bed, and crawled under the covers it was after midnight…not joke. I was too tired to think, much less type.
Overall the day went better than we anticipated it going, I think it was due largely to the fact that we had researched this particular test more than any test Lucy has had… to say that we were prepared would be an understatement. Any test that you have to put your child to sleep to check their anatomy and have the testing mechanism placed, automatically qualifies it as being complicated. I know I have said this before, but anesthesia and mito are not a good combination, add an arrogant anesthesiologist to the situation and now it becomes difficult in addition to being complicated.
Lucy woke up on the wrong side of the bed as usual from anesthesia. She was grumpy and made sure everyone knew it. She was not impressed with the way they taped the manometry catheter and foley,which we used to attach a drainage bag, to her stomach. She is a creature of habit and does not like it when you go and change things on her… at least not before getting her approval first. We try and prepare her as best as possible for what is going to happen when she has anything done to her, experience has taught us this. I guess we assumed that since she has so many tubies attached to her body at all times that these would be no big deal to her. You know that saying, never assume anything…
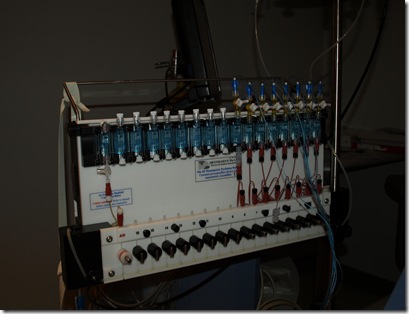
After about an hour we left the PACU and were transferred to the GI suit where Lucy was connected to the maometry machine. I could try and describe it, but I took pictures instead.
The test itself took six hours. Dr. B and I discussed the details of how the study was going to be done a few weeks ahead of time. The first two hours were spent measuring her stomach and small bowel contractions while “fasting”. Lucy was connected to her TPN the entire time due to her severe hypoglycemia. The third hour we clamped her drainage bag so that her stomach would fill with bile and secretions thus simulating “food”. The fourth hour we administered IV erythromycin, a medication used to stimulate contractions in the stomach to help move food. This made Lucy very uncomfortable. She complained of belly pain, was nauseous and retched from the medicine. The fifth hour we unclamped Lucy’s drainage bag and administered octritide, a motility medication used to stimulate the small bowel. Octritide is administered via a shot that you have to place in the leg or arm, not very fun for anyone involved. During the sixth hour an x-ray was taken to check for placement of the manometry catheter, and then we were done with the study.
We arranged for Lucy to have just a g-tube placed after the study. We did this because we knew the IR department at CHOP does not allow parents into the procedure rooms when they place GJ tubes. The IR department at DuPont does, and so we much prefer having our gj-tubes placed at DuPont. Plus after having 12 tubies placed in the IR at DuPont we have developed quite a good relationship with the team there. Lucy’s stoma, the hole in which you insert her tubies, was tight when we went to put in the g-tube, it took quite a few people and attempts to get it in which made for a dramatic end to a very long day. Stoma sites can close fairly quickly, even stomas that are as old as Lucy’s. Because the tubes we used for the study were smaller than Lucy’s typical 16fr diameter tube, her stoma closed in around the other tubes.
Several times throughout the test Dr. B stopped by to see how things were going. At first glance it appears that the study confirms what Drew and I already know, Lucy has slow to no motility. The medications we trialed do not appear to have done anything. Dr. B looked surprised and commented to us that once he interprets all of the data we will need to sit down with Lucy’s current care team and come up with a plan. Drew and I are well of the fact that Lucy’s GI system has been declining, we did not do this study to tell us that. We did this study to see if there was anything we can do to improve her very poor motility. Good or bad we knew that we needed to do this study to rule in or out any possibilities we may have at giving Lucy the best quality of life. We know there is not cure for Lucy at the current time… but we are always going to hold on to hope.












Post Comment
Glad that the test was fairly uneventful! I hope you get the results soon and can get a good sense of your options! Lucy looks darling as always, even grumpy from anesthesia. :)
Post a Comment